The Financial Accountability Office has released the Ford PC government’s funding plans for the various health care sub-sectors. The news is not good. The funding plans for 2022/3 in several key line items are down compared to actual funding in 2021/2: Funding plans for long-term care services are down $26
Continue readingTag: homecare
THE CAREGIVERS' LIVING ROOM A Blog by Donna Thomson: PARENT TO PARENT: Learning to TRANSITION
A few weeks ago, I came across this wonderful piece on transitions by a parent of twins, Marquitha Gilbert. I contacted Marquitha and we had a rich conversation about parenting, writing and the many transitions that we experience with our children over time. I am so grateful to Marquitha for
Continue readingTHE CAREGIVERS' LIVING ROOM A Blog by Donna Thomson: SAFE HIRING OF HOMECARE DURING COVID
JOIN ME AND CO-PRESENTER MIKE GEORGE FOR A VIRTUAL GROUP SESSION ON SAFELY HIRING HOME CARE DURING COVID! DETAILS AND REGISTRATION HERE – Thursday, June 25th at Noon, eastern time Here’s the press release! The COVID-19 pandemic has prompted many frightened family caregivers to assess whether or not it’s safe to
Continue readingDefend Public Healthcare: Cuts drive crisis for unpaid women caregivers
Cascading health care cuts are resulting in significant problems for home care patients and their families, seriously undermining the main defense the government makes for its policy of hospital and long-term care cutbacks. With hospital cutbacks …
Continue readingDefend Public Healthcare: Cuts drive crisis for unpaid women caregivers
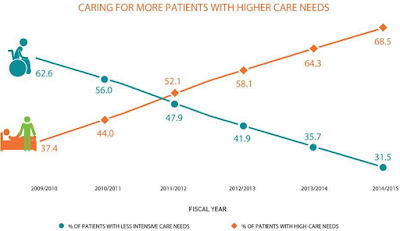
With hospital cutbacks and a virtual freeze on long-term care beds, home care and unpaid caregivers must now take care of sicker and sicker patients. This change in home care has been sudden and dramatic, as demonstrated in the graph below from the the Ontario Association of Community Care Access Centres (the OACCAC represents the public sector organizations which manage home care for the government).
The OACCAC estimates cost pressures of about 5% per year to offset demographic changes and for the absorption of patients that would otherwise have been treated in hospitals or long-term care. The OACCAC adds that funding has fallen short of that level in recent years, reducing care.
- Among patients with moderately severe to very severe impairment in cognitive abilities, 54.5% had caregivers who were distressed.
- When patients needed extensive assistance with or were dependent in some activities of daily living, 48.7% had distressed caregivers.
- When patients were at the two most severe levels of health instability, 56.1% had caregivers who were distressed.
- Those who had Alzheimer’s or other forms of dementia increased to 28.6% from 19.5%
- Those with mild to very severe cognitive impairment increased to 62.2% from 38.1%
- Those experiencing moderate to very severe impairment in ability to perform activities of daily living such as washing their face or eating increased to 44.5% from 27.6%
- Those with slightly to highly unstable health conditions associated with greater risk of hospitalization or death increased to 43.2% from 27.3%
- The patients averaged a year and a half older than in 2009/10, increasing from 77.4 years to 78.9 years.
- On average, patients whose caregivers experienced distress received 31.5 hours per week of care from those caregivers, compared to the 17.1 hours per week received by patients whose caregivers were not distressed.
The home care patients are much sicker than they were only a few years ago, increasing the burden for the unpaid caregivers. The result for the unpaid caregivers — usually women — is increasing distress, anger and depression, with a significant portion unable to continue. More paid hours for PSWs and other home care workers is obviously part of the solution.
The study — released by the government sponsored organization Health Quality Ontario — does not specifically connect this “perfect storm” to the ongoing health care cuts. But it is clear those cuts are driving sicker patients to home care and unpaid caregivers — and now we know those women caregivers are basically being thrown under the bus.
The main government response to the cuts in hospital and long-term care is to suggest that they are doing more in home and community care. This study suggests this response has big problems.
Update May 16, 2017: A new study published by the New England Journal of Medicine and funded by the Canadian Institute of Health Research, the Ontario Academic Health Science Centre, the Ministry of Health, and the University of Toronto also shows major problems for caregivers. Specifically, in this case, very high levels of depression among caregivers (who were mostly women) of patients who survived a critical illness.
THE CAREGIVERS' LIVING ROOM A Blog by Donna Thomson: Regrets and Triumphs in Mothering a Complex Son: A Video Conversation
Recently, I had the privilege of sitting down for a chat with my friend and colleague in disability activism, Jennifer Johannesen. Jennifer is a blogger and the author of “No Ordinary Boy: The Life and Death of Owen Turney”, a riveting memoir of life with her son Owen whose medical
Continue readingTHE CAREGIVERS' LIVING ROOM - A Blog by Donna Thomson: Power Politics: Professional Caregivers in the Family Home
Recently, I gave an interview with Nicole Scheidl, of Fit Minds, a program for enhanced communication between people with dementia and their caregivers. My topic for this interview was the power relationships between paid caregivers and family caregivers in the home setting. I blogged about this topic earlier this year
Continue readingDefending Public Healthcare: Why are fewer hospital patients waiting for LTC?
Ontario hospitals report a significant decline in the number of patients in hospital beds who are waiting for a long term care bed. From November 2009 to March 2013, the number of patients waiting for LTC was reduced by 1,282 patients, an astonishing decline of 41%. This sounds like a
Continue readingTHE CAREGIVERS' LIVING ROOM - A Blog by Donna Thomson: How to Advocate for Care: Part 1
Advocating for care is a complicated task. The job of caregiving does not discriminate on the basis of family income, race, education or employment status. Anyone, anytime can find themselves suddenly thrust into the position of giving care to a loved one. And if the care needs are high, the
Continue readingDefending Public Healthcare: Homecare funding falls short – of even aging cost pressures?
The Ontario government likes to suggest that the planned annual 4% nominal increase in “home and community care” funding will offset their cuts to hospital services and squeeze on long term care beds. But it’s not totally clear that this funding will offset cost pressures on home and community care
Continue readingDefending Public Healthcare: Seniors recommendations head off in wrong direction
The government’s new senior’s “action plan” discussed in the last post follows on from Dr. Samir K. Sinha’s report for the government “Living Longer Living Well”. Sinha’s report is labelled only as “Highlights and Key Recommendations”. A “full report will present considerably more detailed findings and recommendations that will
Continue readingDefending Public Healthcare: More privatization via Liberal "community care"
Health care privatization continues to come to Ontario via the Liberal government’s version of “community care.” Most obviously this comes by moving services from public hospitals to poorly regulated and for-profit retirement homes. …
Continue readingDefending Public Healthcare: Mississauga-Halton gets bigger homecare increase
Another home care funding announcement came out today, this time for Mississauga-Halton.
Mississauga
The news this time was a little better, with a 4.1% funding increase for home care via $5.12 million for the Mississauga-Halton Community Care A…
Continue readingDefending Public Healthcare: Homecare funding finally announced (and it falls short)
The Minister of Health and LTC has finally (7 months into the year) gotten around to making an announcement about the increase to home care funding for this year, at least for the Hamilton Niagara Community Care Access Centre (CCACs fund home care providers). Aside from the long delay, the
Continue readingDefending Public Healthcare: Home care cuts AND hospital cuts
The Chatham-Kent Health Alliance is planning to cut 22 hospital beds to deal with the government’s funding squeeze. The bed cuts are supposed to reduce the hospital’s deficit. The Ontario government has endlessly claimed that improved home care services will offset hospital cuts. “Rebalance” is the Health Minister’s word
Continue reading