Cascading health care cuts are resulting in significant problems for home care patients and their families, seriously undermining the main defense the government makes for its policy of hospital and long-term care cutbacks. With hospital cutbacks …
Continue readingTag: cdnhealth
Defend Public Healthcare: Cuts drive crisis for unpaid women caregivers
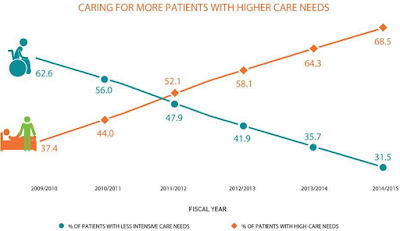
With hospital cutbacks and a virtual freeze on long-term care beds, home care and unpaid caregivers must now take care of sicker and sicker patients. This change in home care has been sudden and dramatic, as demonstrated in the graph below from the the Ontario Association of Community Care Access Centres (the OACCAC represents the public sector organizations which manage home care for the government).
The OACCAC estimates cost pressures of about 5% per year to offset demographic changes and for the absorption of patients that would otherwise have been treated in hospitals or long-term care. The OACCAC adds that funding has fallen short of that level in recent years, reducing care.
- Among patients with moderately severe to very severe impairment in cognitive abilities, 54.5% had caregivers who were distressed.
- When patients needed extensive assistance with or were dependent in some activities of daily living, 48.7% had distressed caregivers.
- When patients were at the two most severe levels of health instability, 56.1% had caregivers who were distressed.
- Those who had Alzheimer’s or other forms of dementia increased to 28.6% from 19.5%
- Those with mild to very severe cognitive impairment increased to 62.2% from 38.1%
- Those experiencing moderate to very severe impairment in ability to perform activities of daily living such as washing their face or eating increased to 44.5% from 27.6%
- Those with slightly to highly unstable health conditions associated with greater risk of hospitalization or death increased to 43.2% from 27.3%
- The patients averaged a year and a half older than in 2009/10, increasing from 77.4 years to 78.9 years.
- On average, patients whose caregivers experienced distress received 31.5 hours per week of care from those caregivers, compared to the 17.1 hours per week received by patients whose caregivers were not distressed.
The home care patients are much sicker than they were only a few years ago, increasing the burden for the unpaid caregivers. The result for the unpaid caregivers — usually women — is increasing distress, anger and depression, with a significant portion unable to continue. More paid hours for PSWs and other home care workers is obviously part of the solution.
The study — released by the government sponsored organization Health Quality Ontario — does not specifically connect this “perfect storm” to the ongoing health care cuts. But it is clear those cuts are driving sicker patients to home care and unpaid caregivers — and now we know those women caregivers are basically being thrown under the bus.
The main government response to the cuts in hospital and long-term care is to suggest that they are doing more in home and community care. This study suggests this response has big problems.
Update May 16, 2017: A new study published by the New England Journal of Medicine and funded by the Canadian Institute of Health Research, the Ontario Academic Health Science Centre, the Ministry of Health, and the University of Toronto also shows major problems for caregivers. Specifically, in this case, very high levels of depression among caregivers (who were mostly women) of patients who survived a critical illness.
Defend Public Healthcare: Ontario hospital length of stay in rapid decline, Canadian average now 21% longer
New hospital inpatient length of stay data published by the Canadian Institute for Health Information (CIHI) indicates [1] Ontario lengths of stay continue to decline, but the pace of decline has picked up, and [2] the gap between the Ontario and Canad…
Continue readingDefend Public Healthcare: Health care employment in Ontario and Canada
Hospital employees in Ontario form a much smaller part of the population than in the rest of Canada – in 2014 about 0.32 % less of the population than in the rest of Canada. As a result, if Ontario had the same percentage of the population as the rest of
Continue readingDefend Public Healthcare: Rapid change in public hospital services
Canadian Institute for Health Information (CIHI) hospital data indicates big changes in hospital activity, particularly in the most recent four years reported. Ontario, especially, is experimenting with hospital cuts and restructuring. Hospital inpatient days are now dropping rapidly in Ontario – with a drop of 13.4% in inpatient days
Continue readingDefending Public Healthcare: Rest of Canada spends 23% more on hospitals than Ontario
Provincial government hospital expenditure per person in Ontario compared to the rest of Canada based on CIHI data. A large gap has grown between what the Ontario provincial government spends on hospitals and what other Canadian provinces spend. Since 2004/5 the gap has grown from a mere $9.43 per person to
Continue readingDefending Public Healthcare: Are hospitals primarily providers of acute care?
Hospitals are often stereotyped as providers of acute care services. In fact, acute care accounts for a relatively small portion of total hospital services. As noted a few days ago, costs per acute care patient (or, more exactly, per “weighted case”) in Ontario are significantly below the national average, coming
Continue readingDefending Public Healthcare: Ontario: 6.1 fewer hours of care per hospital patient
The real costs for the average hospital acute care patient are declining. As noted yesterday this is true for both Ontario and Canada, based on data just released from the Canadian Institute for Health Information. But the CIHI data also revealed other interesting trends, likely related. Administrative Costs Decline: Administrative costs continue their long
Continue readingDefending Public Healthcare: Costs of hospital treatment falling
Ontario has the lowest hospital cost per weighted case of all the provinces. And the cost difference between Ontario and the rest of the country is growing. Hospital Cost Per Weighted Case ($) 2009-2010 2010-2011 2011-2012 Newfoundland 6,001 6,283 6,332 PEI DQ DQ 5,257 Nova Scotia 4,998 5,403 5,384 New
Continue readingDefending Public Healthcare: Are employer paid drug plans unsustainable?
A Great West Life Assurance executive recently claimed that private insurance for drug plans was becoming unsustainable — unless changes are made. Almost all private drug insurance plans are paid through employer paid insured benefit plans (often bargained with trade unions). In fact, although there were significant increases during the
Continue readingDefending Public Healthcare: Health care spending continues decline
Contrary to the hysteria from conservatives, health care spending continues to decline as a percentage of the provincial budget. Last year, health care accounted for 38.5% of total expenditures, this year the government plans to bring it down to 38.3%. This continues the trend downwards since 2003/4 when health care
Continue readingDefending Public Healthcare: English reforms lose their appeal in Ontario?
England has had a disproportionate impact on health care reform in Ontario over the last decade or so –under both Liberal and Progressive Conservative governments. After the election of a Conservative-Liberal Democrat government in Britain in 2010, English health policy took a decided turn towards bonzo-privatization. As elsewhere, the electorate
Continue readingDefending Public Healthcare: Nursing levels low and getting lower
Yesterday, I wrote about the significant lack of nursing care in Ontario hospitals compared to the other provinces. Even on a Canada-wide basis, there was 5.32 hours more nursing care per patient than in Ontario in 2010-11 (year end March 31). That sounds kind of shocking. But it looks
Continue readingDefending Public Healthcare: Hospital costs lower in Ontario
The “cost per weighted case” in Ontario hospitals in 2010-11 was $5,143, according to a new report from CIHI. (This indicator measures the relative cost-efficiency of a hospital’s ability to provide acute inpatient care.) The Ontario cost per weighted case compares with a Canada-wide average of $5,230.96. In other words, the Canada-wide
Continue readingDefending Public Healthcare: MRSA and C. Difficile rates fall (but not here)
A new report from the Chief Medical Officer of Health in England reports that “rates of C. difficile have fallen consistently in all English regions in recent years. MRSA has fallen markedly and is now very low in many areas.” As noted in November, there is no evidence of that in Ontario, as
Continue readingDefending Public Healthcare: Hospital cuts in 1.7% to 2.7% range
More hospital savings. Joanna Frketich reports Hamilton Health Sciences needs to find $20 million to $25 million in savings, while Hamilton St. Joseph’s is cutting $10 million to $12 million, and Burlington’s Joseph Brant must cut $4 million. In total, $34 to $41 million in cuts for Hamilton area hospitals.
Continue readingDefending Public Healthcare: It’s raining cuts
Premier designate Kathleen Wynne has strongly suggested that hospital cutbacks will continue Of the cuts just announced at the Ottawa Hospital, Wynne says the government is “transforming the health-care system, so services that need to be delivered in a hospital setting are delivered in a hospital setting, but services that don’t are
Continue readingDefending Public Healthcare: A tiny response to growing elder needs
The Ontario government’s 26 page Action Plan for Seniors came out yesterday. There’s not much to it. About half of the report simply rehashes what is already in place. To the good, they at least formally recognize that the elderly population is expanding rapidly and that this is going to require
Continue readingDefending Public Healthcare: Major decline in nursing in Ontario hospitals
There was a sharp reduction in the number of Registered Nurses (RNs) working in Ontario hospitals in 2011, with a cut of 2,750 RNs to 58,699 according to new CIHI data. That’s a 4.47% decrease in one year. Community health numbers also took a very hard hit, while numbers were up very
Continue readingDefending Public Healthcare: No progress on hospital superbugs
There has been no progress stopping the spread of superbugs in Ontario hospitals according to government data.
Reported C. difficile rates are about the same as they have been, starting this past year at 0.35 cases per thousand patient days…
Continue reading